Sciatica-Ask The Experts Part II
“Sciatica” is an often misunderstood term that is used to describe a host of conditions related to pain in lower back, hip, and leg. To get to the heart of this issue, I recently spoke with local expert, Dr. Rajan Perkash.
Dr. Perkash is an M.D. specializing in an area known as Physical Medicine and Rehabilitation (PM&R). His speciality also goes by the term Physiatrist.
In addition to being an expert diagnostician with well over 20-years of experience in the field, Dr. Perkash is also Board-certified in Pain Medicine.

I asked Dr. Perkash to address some of the most common questions people have about sciatic nerve pain. Here’s what he had to say.
TR: What is sciatica and why does is happen?
RP: “Sciatica” is a term used to describe pain radiating from the buttock down the leg.
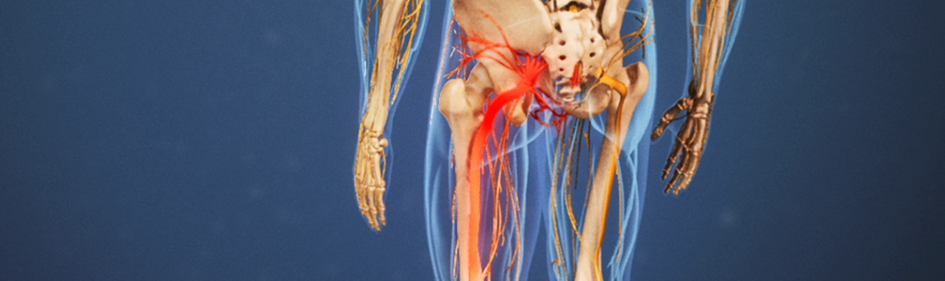
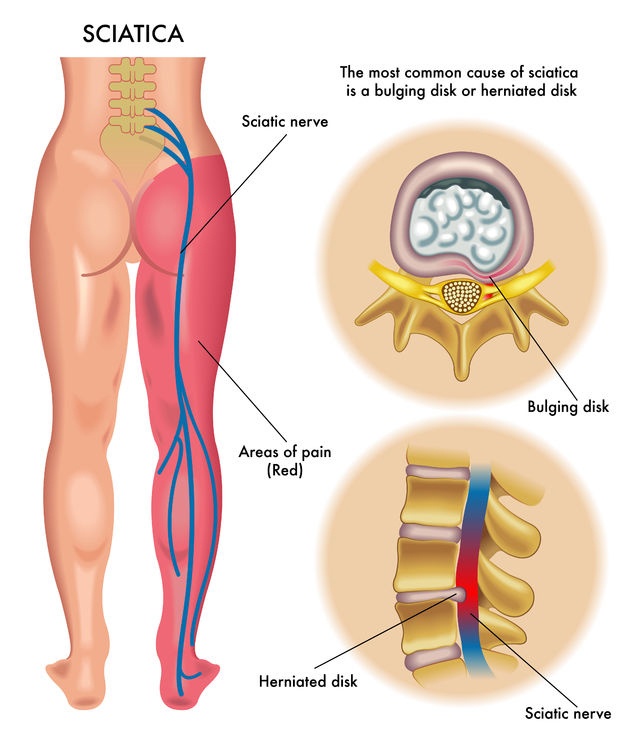
The most common reason for “sciatica” symptoms is a disc disruption in the lower lumbar spine with irritation of the nearby L5, S1, or possibly L4 nerve roots. These are the nerve roots that coalesce to form the Sciatic Nerve in the gluteal region.
TR: Can other conditions ‘look’ like sciatica?
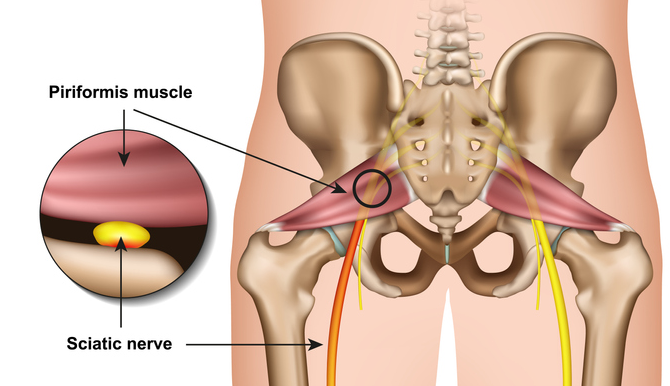
RP: People can have similar symptoms of pain due to sacroiliac joint dysfunction, piriformis syndrome, gluteal strain injuries, trochanteric or ischiogluteal bursitis, or other conditions affecting the buttock or posterior thigh.
Differentiating between these diagnoses requires a careful history of the symptoms, a thorough physical examination, and potentially correlating imaging findings such as an MRI of the lumbar spine with the history and physical examination findings.
TR: How is an x-ray different from an MRI?
RP: X-rays or “Roentograms” show dense tissues such as bones or other calcium rich tissues. It does not show soft tissues such as nerves, intervertebral discs, muscles, or ligaments well.
An MRI, or Magnetic Resonance Imaging, shows both ‘hard’ and ‘soft’ tissues such as bones and muscles by using a very strong magnet to orient the protons, or positively charged elements of each tissue and then collecting that information in an image.
MRI scans are used to assess three-dimensional views of tissues by utilizing various orientations of two-dimensional tissue planes.

TR: When are X-rays more useful? How about MRIs?
RP: MRIs are very useful for assessing more detailed anatomy of both soft and hard tissues in three dimensions. X-rays involve radiation exposure and are relatively inexpensive, while MRI scans only involve magnetic fields and no radiation, but are considerably more expensive.
Fractures of bones are often seen easily on X-rays, while soft tissue disruptions such as a disc herniation are [more easily] visualized on an MRI scan.
TR: OK, let’s talk about treatment. When should a patient try conservative therapies like P.T. or acupuncture vs. an epidural injection?
RP: If a patient has a disc herniation with symptoms of “Sciatica” (i.e. radicular low back pain), and they have not improved with an initial trial of oral medications and potentially physical therapy for a few weeks, or if their pain is debilitating preventing even normal activities or a trial of physical therapy, then epidural steroid injections can be implemented to reduce pain and inflammation to create a better healing environment and facilitate the patient’s rehabilitation and exercise program.
In most cases oral medications, physical therapy, acupuncture, and other more conservative treatments can lead to improvement and resolution of symptoms without the need for epidural injections.
TR: What is an epidural injection?

RP: Epidural steroid injections are injections of corticosteroid (e.g. “Cortisone”) into the epidural space—a space between the intervertebral discs in the spine and the nearby exiting nerve roots.
Sometimes when disc material comes in contact with nerve roots, the situation creates inflammation and subsequently pain down the leg in the distribution of the nerve root that is inflamed or irritated.
TR: How does it work and what outcome can patients expect?
RP: The injections can lead to a more rapid return of functioning, healing, and resumption of activities of daily living and recreational activities. By reducing pain and inflammation, the patient is able to more easily participate in a Rehabilitation/Physical Therapy exercise program to learn exercises that should be done long term to reduce the risk of future problems.
TR: What role does exercise play with regard to a patient’s recovery?
RP: With a long term home exercise program, most patients can make a full recovery with long term excellent results. Most patients who keep up their home exercises can function without limitations long term with little or no pain.
Epidural injections are only a part of the treatment program, with long term lifestyle changes and a daily exercise program for core strengthening, lower extremity flexibility, and cardiovascular fitness being most important for long term success and functioning.

TR: If you could describe the perfect rehabilitation program, what key elements would you include?
RP: I find that a combination of core stabilization exercise plus regular cardiovascular exercises allows for maximum functioning, minimizing pain, and promoting longevity of spine and general health.
Cardiovascular exercise releases endorphins (i.e. endogenous opioids) in our brain and spinal cord that actually reduce overall body pain—often known as the “Runner’s High.”
In addition, cardiovascular exercise increases blood flow to the musculoskeletal system and neurological system. I have found swimming in particular to be outstanding as an adjunct cardiovascular exercise for unloading the spine and joints and allowing our aging bodies to have a very therapeutic environment to minimize joint and musculoskeletal pain.

TR: Any final thoughts on the subject?
RP: All of us will have aching joints and spinal pain at one time or another. Those that have a healthy diet, sleep well, and participate in regular cardiovascular and core exercises have much better odds in terms of quality of life, less pain, and overall success in functioning in the activities that matter to them.
TR: Thank you!
About Dr. Rajan Perkash
Dr. Raj Perkash has been treating patients with complex Spine and Sports injuries for the past 22 years at the Palo Alto Medical Foundation. He is Board Certified in Physical Medicine and Rehabilitation and Subspecialty Board Certified in Pain Medicine. He is avidly enjoys a variety of sports and exercise activities, and believes that regular exercise is one of the keys to a happy, healthy life. He has served on the Board of Directors of the Palo Alto Foundation Medical Group for the past 8 years.